Créez votre propre collecte de dons !
filtrer
Par pays
- Par pays
- Afghanistan
- Crise Ukrainienne
- Bangladesh
- Bulgarie
- Burkina Faso
- Colombie
- Côte d’Ivoire
- Égypte
- Éthiopie
- France
- Irak
- Liban
- Madagascar
- Malaisie
- Mexique et Amérique Centrale
- Myanmar
- Népal
- Nigeria
- Palestine
- Pakistan
- Philippines
- République centrafricaine
- République démocratique du Congo
- Russie
- Sud-Caucase
- Syrie
- Tanzanie
- Yémen
Par action
Réinitialiser les filtres

Articles
12.04.2024
Adoption du Pacte européen sur l’asile et la migration : une dramatique opportunité manquée ?
Après 4 ans de négociations, le Pacte européen sur l’asile et la migration a été adopté à une courte majorité par les eurodéputés avant d’être transmis aux Etats membres du Conseil pour un vote à venir à la majorité qualifiée.

Articles
15.04.2024
Famine dans la Corne de l’Afrique : notre intervention

Articles
03.04.2024
Action internationale pour protéger les civils à Rafah : il sera bientôt trop tard
Il y a une semaine, le Conseil de sécurité de l’ONU adoptait une résolution exigeant un cessez-le-feu immédiat, et quelques jours après, la Cour internationale de justice (CIJ) indiquait deux mesures additionnelles conservatoires dans le cadre de la plainte pour génocide déposée contre Israël par l’Afrique du Sud. Alors que les attaques s’intensifient, 13 organisations humanitaires et de droits humains lancent l’alerte ; les États doivent agir sans plus attendre afin de garantir l’application de cette résolution et empêcher la perpétration de crimes atroces à Rafah.

12
Mars.
Agenda
Table ronde - Comment renforcer la protection des personnels humanitaires ?

Articles
12.02.2024
La 9ème édition de la Journée Scientifique de Médecins du Monde
Médecins du Monde organise la neuvième édition de la Journée Scientifique de la Santé Humanitaire et Solidaire le jeudi 4 avril 2024 à l’Auditorium du Monde, 67-69 avenue Pierre Mendès-France, Paris 13ème.
11
Mars.
Agenda
Réunion d'information bénévoles - Angoulême

19
Mars.
Agenda
Réunion d'information bénévoles - Marseille

Articles
02.04.2024
Dix ONG appellent l’UE à agir pour empêcher la famine à Gaza
ActionAid et neuf ONG internationales appellent l’UE à agir sans plus attendre pour éviter la famine à Gaza. Dans une lettre ouverte, les organisations appellent l’Union européenne à adopter quatre mesures, notamment en plaidant pour un cessez-le-feu immédiat et permanent et la fin des transferts d’armes vers Israël.

Articles
27.03.2024
Fin de la trêve hivernale : Médecins du Monde se mobilise dans plusieurs villes de France
Alors que la trêve hivernale touche à sa fin dans quelques jours, Médecins du Monde se mobilise partout en France pour alerter sur la hausse sans précédent du nombre de personnes vivant à la rue et des conséquences sur leur santé.

5
Déc.
Agenda
Webinaire - S'engager chez Médecins du Monde - 5 décembre 2023
Articles
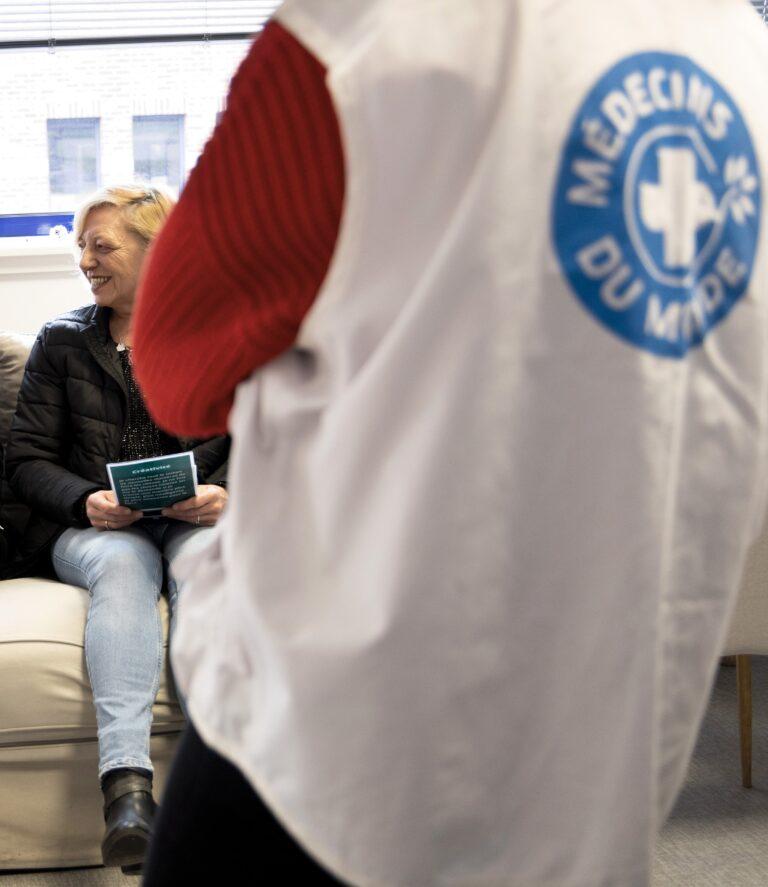
25.03.2024
JOP Paris 2024 : les droits humains ne sont pas respectés
Alors que l’ouverture des Jeux olympiques et paralympiques de Paris 2024 approche à grands pas, le nettoyage social en cours qui invisibilise les populations les plus précaires s’intensifie.

Articles
14.03.2024
Le grand entretien avec Didier Fassin et Anne-Claire Defossez
Didier Fassin, médecin et anthropologue, professeur au Collège de France, et Anne-Claire Defossez, sociologue et chercheuse à l’Institute for Advanced Study de Princeton, ont enquêté sur les enjeux humains et politiques qui se jouent. Sur l’espoir qui demeure et les mécanismes solidaires qui se mettent en place malgré la répression obstinée des forces de l’ordre.
Découvrez les reportages
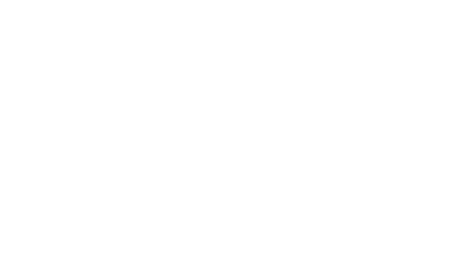
Médecins du Monde
Ils parlent de Médecins du Monde
-

De retour de Rafah, la responsable du Moyen-Orient pour l’ONG Médecins du monde témoigne de la situation sur place
14.03.2024DécouvrirUrgences et crises -
SpeeDons : plus de 2 millions d’euros récoltés au marathon de jeux vidéo
04.03.2024DécouvrirCollecte -
« Femmes SDF, sans toit, ni droits »
02.03.2024DécouvrirMal-logement